Introduction
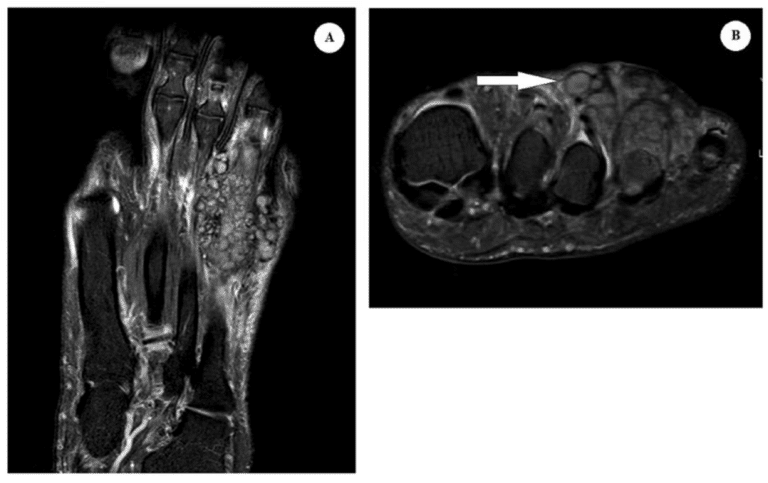
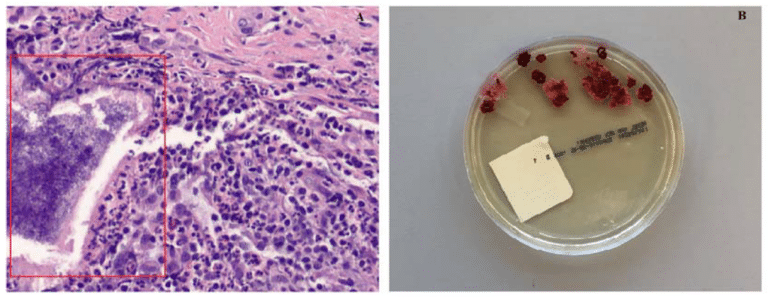
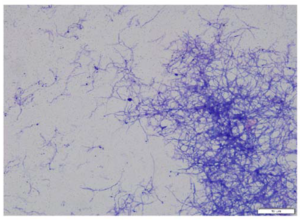
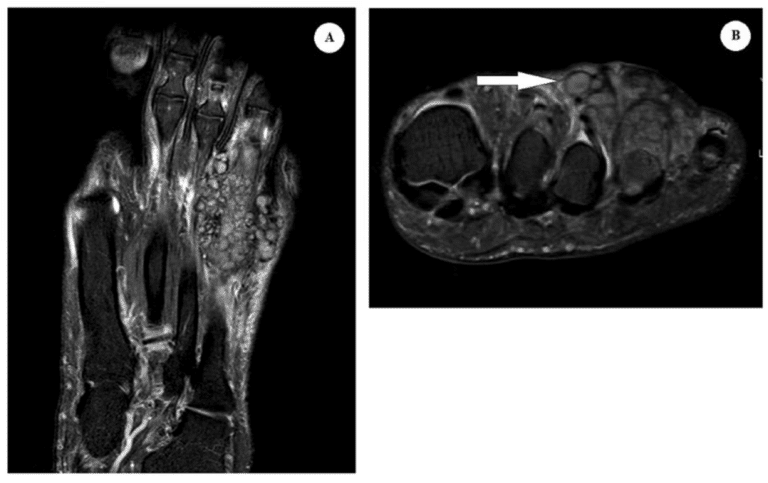
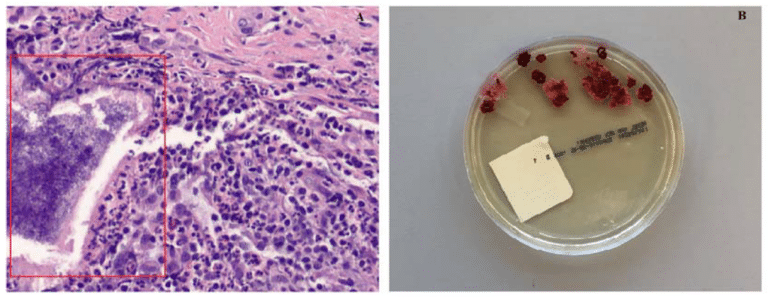
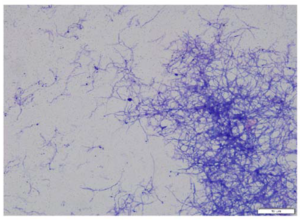
A 50-year-old Nigerian woman presented to the infectious diseases clinic for evaluation of incidental left foot mass. The patient is a healthcare worker who first sought medical attention after a large battery was accidentally dropped on her foot. Her past medical history is significant for removal of a “cyst” in the same area of her foot seven years ago in Nigeria, after presenting with progressive swelling. Aside from mild swelling and discomfort while wearing tight fitted shoes, she remained asymptomatic until the day of battery trauma. Following her accident, she was seen by an orthopedic surgeon for severe left foot pain and swelling. Magnetic Resonance Imaging (MRI) of the left foot revealed a 1.8 × 3.4 × 4.4 cm infiltrative multicystic mass along the dorsal aspect of the fourth metatarsophalangeal joint that was encasing the overlying extensor tendon (Figure 1). The patient underwent open biopsy of the mass which revealed granulation tissue with evidence of acute and chronic inflammation on histology; Gomori Methenamine-Silver and Fite stains did not show any microorganisms, but sulfur granules were present (Figure 2A). Fungal culture plated onto Sabouraud Dextrose agar had organism growth after 16 days of incubation at 30 °C in ambient air (Figure 2B). Additional staining with Kinyoun and modified Kinyoun staining showed non-acid fast filamentous branching bacilli (Figure 3).
Diagnosis: Actinomycetoma with Actinomadura species
Actinomycetoma is caused by microorganisms of the order Actinomycetales, which includes Nocardia, Actinomadura and Streptomyces species [1]. Actinomadura species are aerobic slow-growing Gram-positive filamentous bacteria found in soil. These organisms are most commonly encountered in the tropical and subtropical regions. Infection with Actinomadura species usually develops after traumatic inoculation of the skin and spread through draining lymphatics. Chronic, progressive granulomatous infections and sinus tracts may form in the subcutaneous tissue of the lower extremities and feet [1,2]. Within the sinus tracts, the bacteria aggregate into granules and evade the innate immune system’s attempts to engulf and inactivate these organisms [1]. In immunocompromised hosts, opportunistic disseminated infection can also occur [3].
Diagnosis of Actinomadura mycetoma is often delayed due to its indolent and chronic course and can often be mistaken for malignancy. The organism can be identified by direct examination as macroscopic granules may be seen with the naked eye. Grains produced by Actinomadura madurae are white, yellow, or cream colored, whereas grains from Actinomadura pelletieri are red [1,4]. The bacteria can be cultured in Lowenstein-Jensen medium or Sabouraud dextrose agar at room temperature. Histopathologic section with hematoxylin-eosin stain can detect grains with a surrounding cluster of neutrophils (Figure 2A). Kinyoun and modified Kinyoun stains are both negative for acid-fastness and demonstrate thin filamentous branching bacilli (Figure 3). Polymerase chain reaction detection and sequencing of 16S rRNA directly from tissue specimens may also aid in diagnosis [5]. Standard radiographic studies such as plain film X-ray can reveal bony involvement such as periosteal erosion and changes consistent with osteomyelitis [1]. A ‘dot in a circle sign’ is usually a characteristic MRI finding seen with this chronic infection (Figure 1) which is described as a sign of a small round- to oval shaped T2-weighted hyperintense lesion with surrounding low-signal intensity and a central low-signal dot [6].
Long term antibiotics is the recommended treatment for chronic actinomycetoma infection. Trimethoprim-sulfamethoxazole (TMP-SMX) is the treatment of choice with an estimated cure rate of 60 percent for uncomplicated cases [7]. Other antibiotic options may include aminoglycosides (streptomycin, amikacin), carbapenems (meropenem, imipenem), dapsone, quinolones, amoxicillin-clavulanic acid, and tetracyclines based upon susceptibilities [7,8]. Antimicrobial susceptibility testing for Actinomadura spp. is not routinely performed in most microbiology labs. In a study of 42 isolates of Actinomadura madurae species referred to the Centers for Disease Control and Prevention, there was no resistance to amikacin, ceftriaxone or imipenem, and 87 percent susceptibility to TMP-SMX alone [9]. Linezolid can be another potential treatment option for those who do not respond to conventional treatment regimens with significant in vitro activity against Actinomadurae spp. and Nocardia spp. [10]. Osteoarticular involvement and disseminated cases may require combination therapy; successful treatment has been described with TMP-SMX and amikacin [7]. Surgery can often be avoided with better prognosis in patients with early diagnosis with appropriate medical management and effective antimicrobial therapy [8]. In developing countries with higher disease prevalence, proper footwear can help prevent direct inoculation of microorganisms.
In our patient, Actinomadura species was identified from the fungal tissue culture after four weeks of incubation and susceptibility results were available after additional three weeks. She was started on oral amoxicillin-clavulanic acid 500 mg three times a day and doxycycline 100 mg two times a day for an anticipated duration of six to twelve months. Rifampin was also added for suspected in vitro activity [7,11] and dual treatment of latent Mycobacterium tuberculosis complex infection. Four weeks after starting antibiotic therapy, she had significant improvement of her symptoms with reduced swelling of the foot.
Funding
There is no relevant funding.
Conflicts of Interest
The authors have no reported conflicts of interest.
References
- Hospenthal, D.R. Agents of Mycetoma. In Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases, 9th ed.; Bennett, J.E., Dolin, R., Blaser, M.J., Eds.; Elsevier: Philadelphia, PA, USA, 2020. [Google Scholar]
- Rosenberg, A.E.; Kattapuram, S.V.; Nielsen, G.P. Infection of Bone. In Diagnostic Pathology of Infectious Disease, 2nd ed.; Kradin, R.L., Ed.; Elsevier: Philadelphia, PA, USA, 2018. [Google Scholar]
- McNeil, M.M.; Brown, J.M.; Scalise, G.; Piersimoni, C. Nonmycetomic Actinomadura madurae infection in a patient with AIDS. J. Clin. Microbiol. 1992, 30, 1008–1010. [Google Scholar] [CrossRef] [PubMed]
- Bravo, F.G.; Arenas, R.; Sigall, D.A. Actinomycosis, Nocardiosis, and Actinomycetoma. In Fitzpatrick’s Dermatology, 9th ed.; McGraw-Hill: New York, NY, USA, 2019. [Google Scholar]
- Salipante, S.J.; Sengupta, D.J.; Hoogestraat, D.R.; Cummings, L.A.; Bryant, B.H.; Natividad, C.; Thielges, S.; Monsaas, P.W.; Chau, M.; Barbee, L.A.; et al. Molecular Diagnosis of Actinomadura madurae Infection by 16S rRNA Deep Sequencing. J. Clin. Microbiol. 2013, 51, 4262–4265. [Google Scholar] [CrossRef] [PubMed]
- Laohawiriyakamol, T.; Tanutit, P.; Kanjanapradit, K.; Hongsakul, K.; Ehara, S. The “dot-incircle” sign in musculoskeletal mycetoma on magnetic resonance imaging and ultrasonography. SpringerPlus 2014, 3, 671. [Google Scholar] [CrossRef]
- Welsh, O.; Vera-Cabrera, L.; Welsh, E.; Salinas, M.C. Actinomycetoma and advances in its treatment. Clin. Dermatol. 2012, 30, 372–381. [Google Scholar] [CrossRef]
- Tight, R.R.; Bartlett, M.S. Actinomycetoma in the United States. Clin. Infect. Dis. 1981, 3, 1139–1150. [Google Scholar] [CrossRef]
- McNeil, M.M.; Brown, J.M.; Jarvis, W.R.; Ajello, L. Comparison of species distribution and antimicrobial susceptibility of aerobic actinomycetes from clinical specimens. Rev. Infect. Dis. 1990, 12, 778–783. [Google Scholar] [CrossRef]
- Patra, S.; Senthilnathan, G.; Ramam, M.; Arava, S.; Bhari, N. Linezolid: A novel treatment option for the treatment of a non-responsive case of actinomycotic mycetoma. Indian J. Dermatol. Venereol. Leprol. 2021, 87, 455. [Google Scholar] [CrossRef]
- Damle, D.K.; Mahajan, P.M.; Pradhan, S.N.; A Belgaumkar, V.; Gosavi, A.P.; Tolat, S.N.; Gokhale, N.R.; Mhaske, C.B. Modified Welsh regimen: A promising therapy for actinomycetoma. J. Drugs Dermatol. 2008, 7, 853–856. [Google Scholar]

