Abstract
Background: The surge of COVID-19 hospitalizations in January 2022, at the onset of the Omicron period and before widespread population immunity, was a window in which to study the impact of vaccination status and other factors on disease severity in Omicron infections.
Methods: This was a case-control study of adults hospitalized with COVID-19 during January 2022 that evaluated risk factors for severe disease. Cases were patients with severe COVID-19, defined in three ways: (1) requiring supplemental oxygen > 24 hours if not on home oxygen, (2) requiring high-level oxygen: either high flow of > 15 L/min, noninvasive ventilation, or mechanical ventilation (MV), and (3) the composite of MV or hospital death. Controls were patients hospitalized with COVID-19 who did not meet the respective case definition.
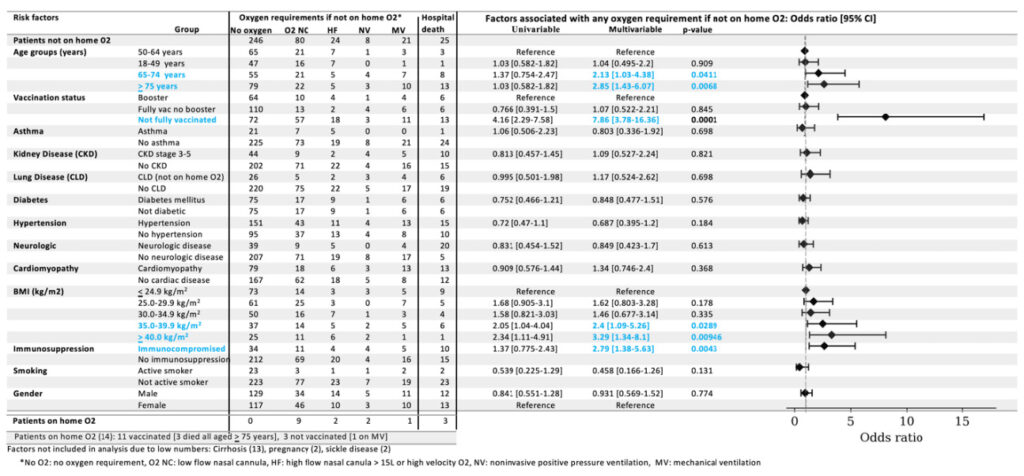
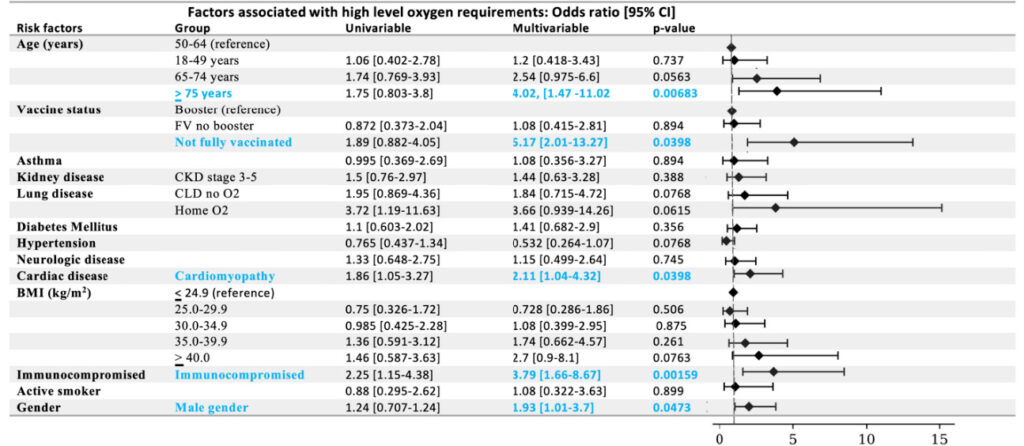
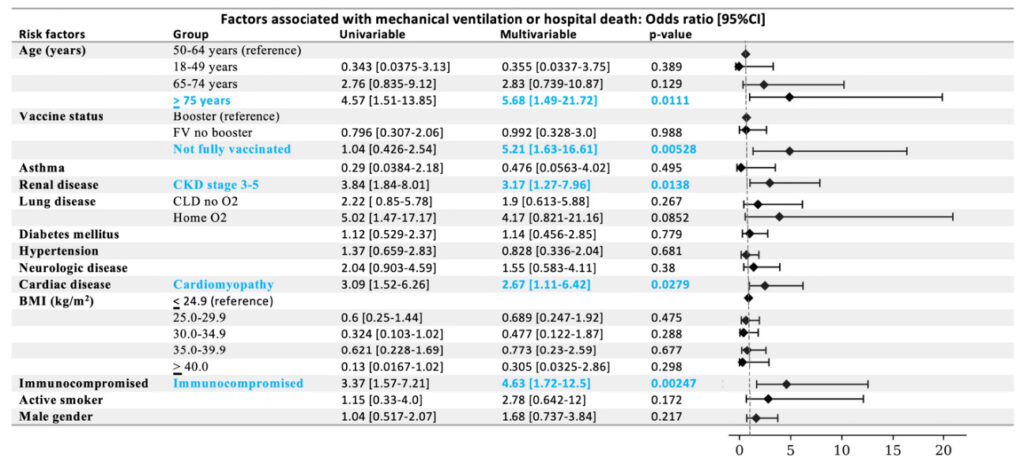
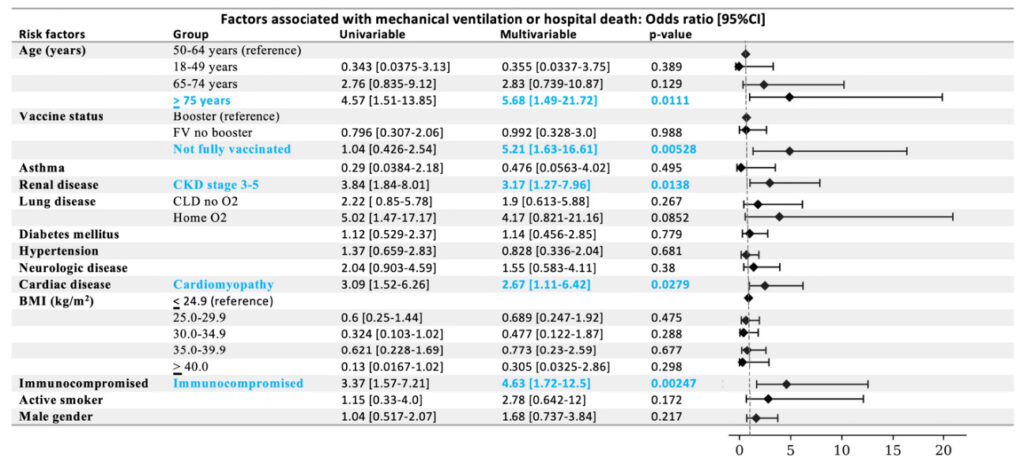
Results: Among the 379 patients not on home oxygen before admission, 133 required supplemental oxygen. Among all 393 patients meeting the study criteria, 58 required high-level oxygen, 22 required MV, and 28 died. Factors associated with all case definitions were (1) absence of full vaccination compared to booster vaccination: requiring oxygen, odds ratio [OR], 7.86 [95% CI, 3.78-16.4]; high-level oxygen, OR, 5.17 [95% CI, 2.01-13.3]; MV or hospital death, OR, 5.21 [ 95% CI, 1.63-16.6]; (2) immunocompromised status: requiring oxygen, OR, 2.79 [95% CI, 1.38-5.63]; high-level oxygen, OR, 3.79 [95% CI 1.66-8.67]; MV or hospital death, OR 4.63 [95% CI 1.72-12.5], and (3) age ≥ 75 years compared to 50 to 64 years: requiring oxygen, OR 2.85, [95% CI 1.43-6.07]; high-level oxygen, OR 4.02 [95% CI 1.47-11.0]; MV or hospital death, OR 5.68 [95% CI 1.49-21.7]. Other factors associated with requiring oxygen were obesity: body mass index (BMI) 35.0-39.9 kg/m2, OR, 2.4 [95% CI 1.09-5.26]; BMI ≥ 40.0 kg/m2, OR, 3.29 [95% CI 1.34-8.10] compared to BMI ≤ 24.9 kg/m2; and age 65-74 years compared to 50-64 years, OR, 2.13 [ 95% CI 1.03-4.38]. Factors associated with requiring high-level oxygen were cardiomyopathy, OR, 2.11 [95% CI 1.04-4.32], and male gender, OR 1.93 [95% CI 1.01-3.7]. Factors associated with MV or hospital death were cardiomyopathy, OR, 2.67 [ 95% CI 1.11-6.42], and chronic kidney disease, OR, 3.17 [95% CI 1.27-7.96]. Factors not associated with any case definitions were full vaccination without compared to with a booster: requiring oxygen, OR, 1.07 [95% CI 0.522-2.21], high-level oxygen, OR, 1.08 [0.415-2.81], MV or hospital death, OR 0.992 [0.328-3.0]; age 18-49 years compared to 50-64 years: requiring oxygen, OR, 1.04 [95% CI 0.495-2.2]; high-level oxygen, OR, 1.2 [95% CI 0.418-3.43]; MV or hospital death, OR, 0.355 [95% CI 0.034-3.75]; and other medical conditions.
Conclusions: In patients hospitalized with COVID-19 during the Omicron surge of January 2022, factors associated with requiring oxygen were the absence of full vaccination, immunosuppression, age ≥ 65 years, and body mass index ≥ 35 kg/m2, but not the absence of a booster if fully vaccinated. This is further evidence that immune memory mitigates disease severity in Omicron infections.
Introduction
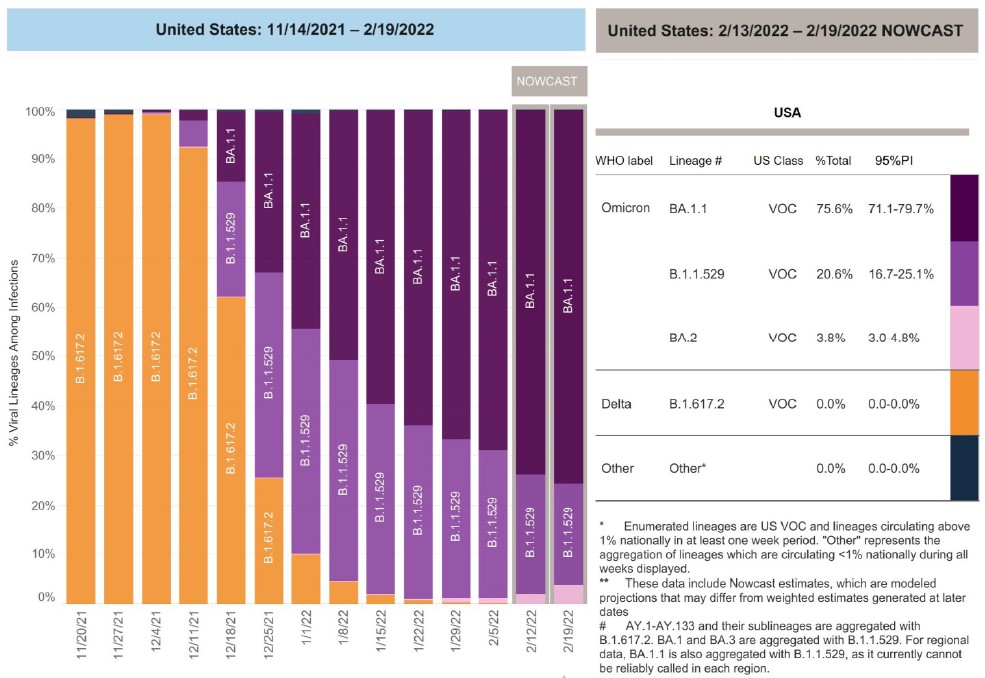
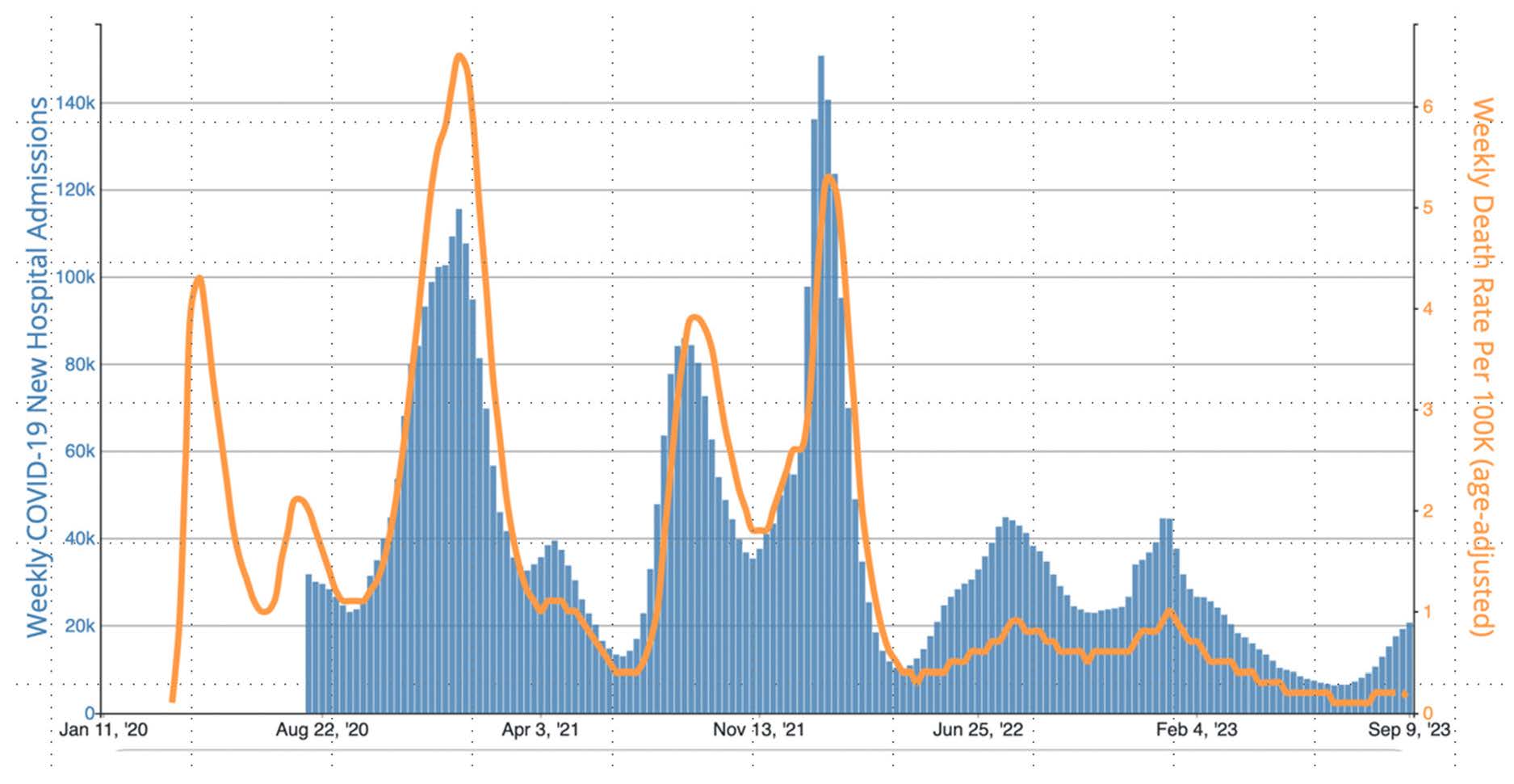
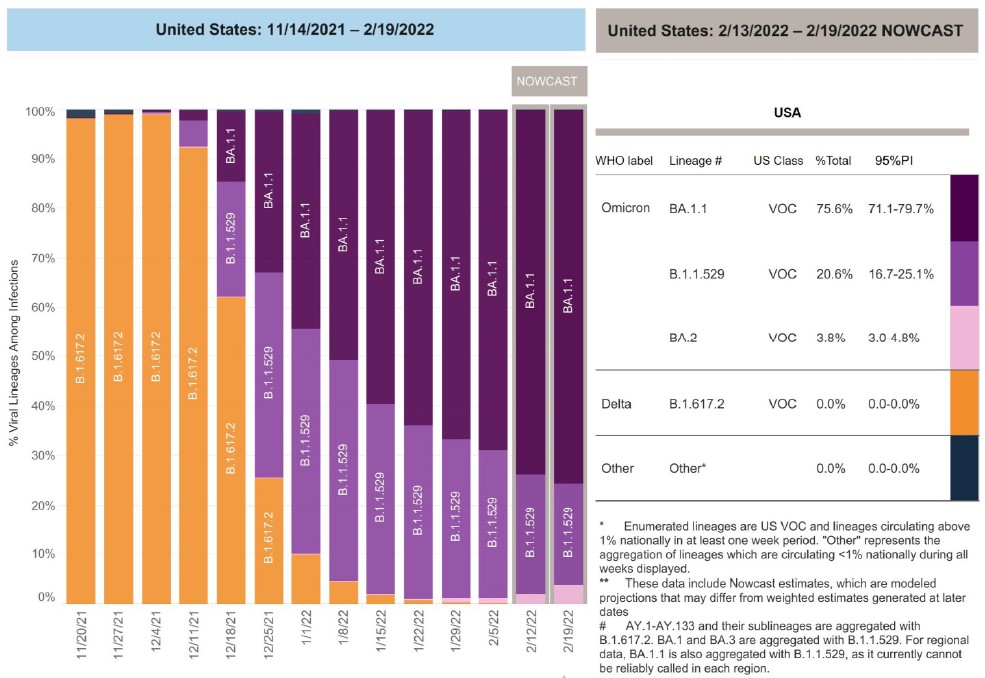
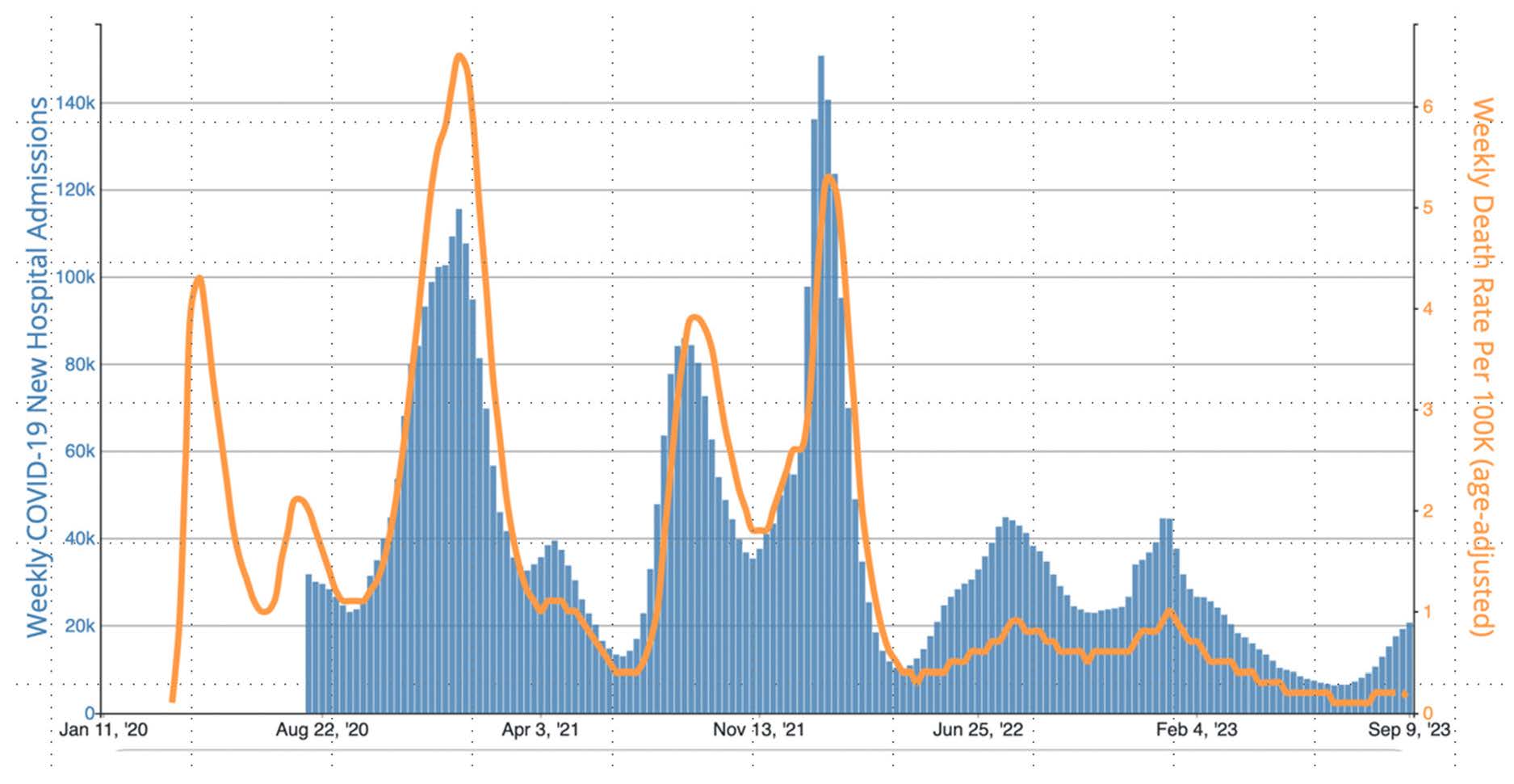
The Omicron variant of SARS-CoV-2, B.1.1.529, was first recognized in South Africa and reported to the World Health Organization (WHO) on November 24, 2021. Changes in key regions of the spike protein allowed it to escape immunity from past infection and diminish effectiveness of COVID-19 vaccines that targeted the ancestral strain spike protein. In the United States in December 2021, the Omicron subvariants B.1.1.529 and BA.1.1 replaced Delta B.1617.2 as the predominant variants, rising to > 75% of new weekly cases on December 25, 2021, and > 95% on January 8, 2022 (Figure 1). From December 2021 through January 2022, there was a surge of COVID-19 cases and hospitalizations in the United States, surpassing previous records (Figure 3) [1].
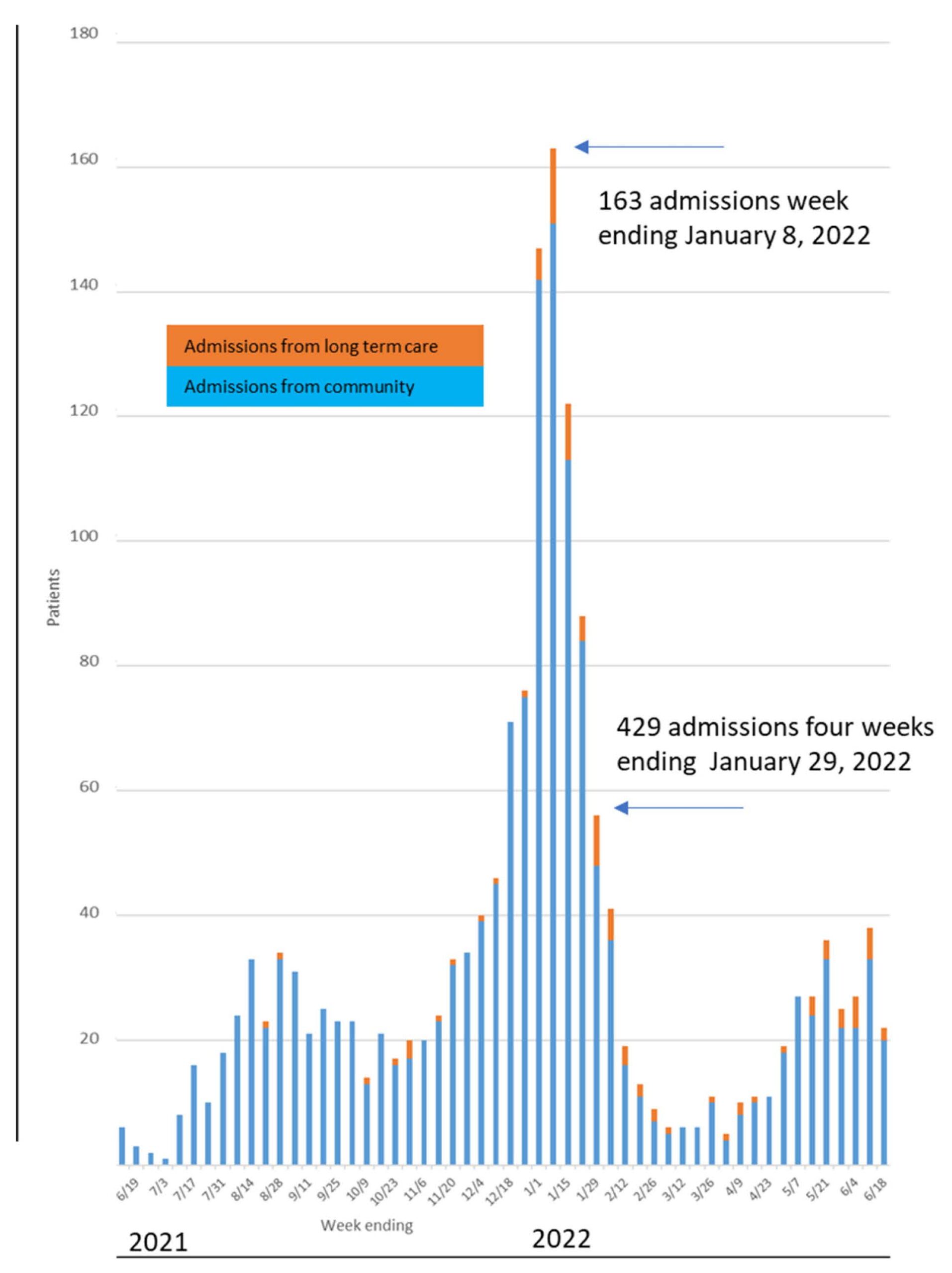
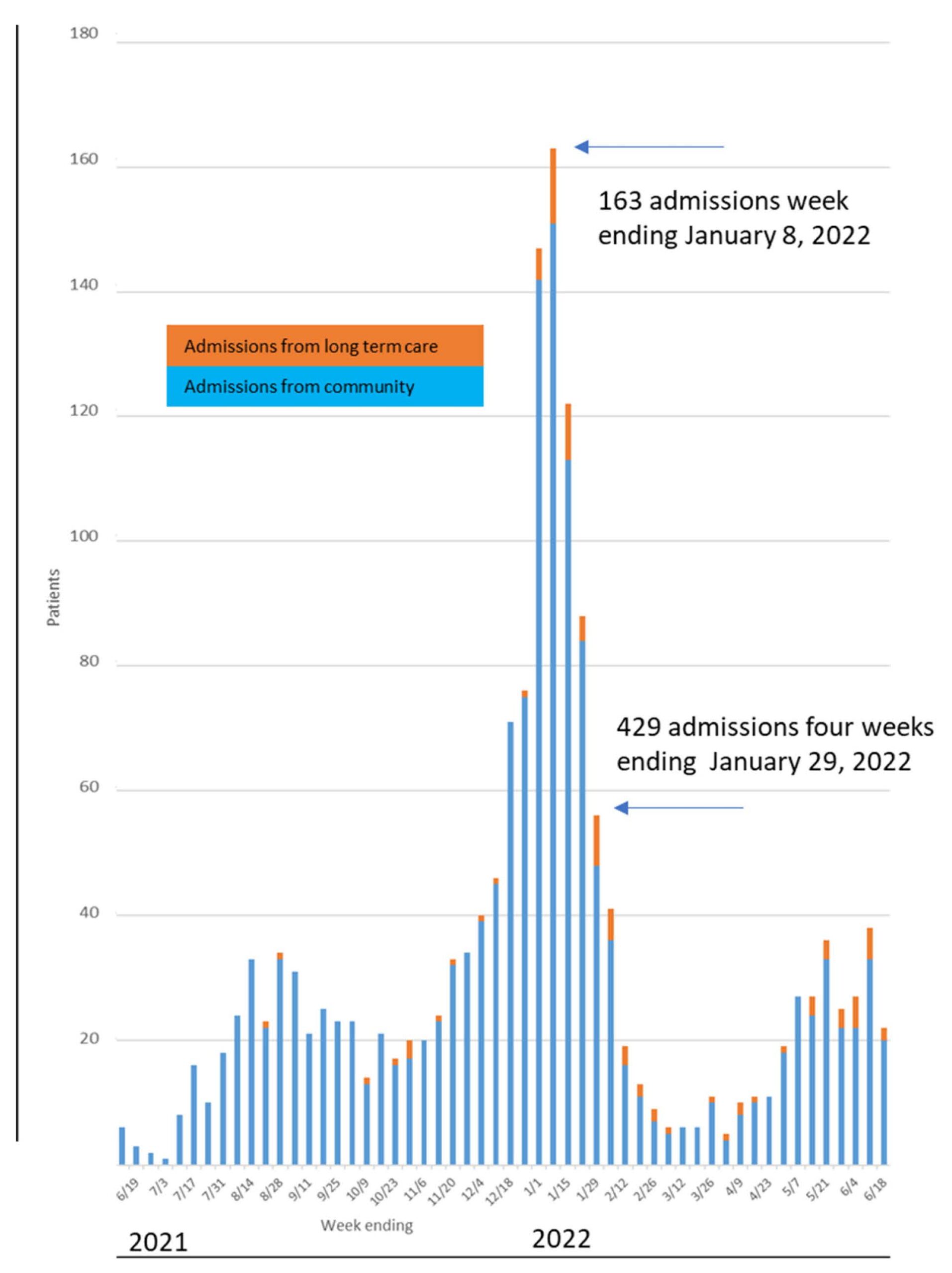
Edward Hospital is a 359-bed community hospital in Naperville, Illinois, that predominantly serves residents of DuPage and Will counties. Edward Hospital admitted 429 patients with COVID-19 during the 4 weeks ending January 29, 2022 (Figure 2). In this study, we evaluated cases of severe COVID-19 disease, as measured via oxygen requirements and hospital survival, in patients admitted to Edward Hospital during January 2022 and their association with vaccination status, age, immunosuppression, and other medical conditions.
Background
There were 163 patients admitted with COVID-19 to Edward Hospital in the week ending January 8 and 429 admitted over the four weeks ending on January 28, 2022. All patients admitted to the hospital were required to be tested for SARS-CoV-2 if they had not been recently positive prior to admission. During January 2022, 38% of admitted patients tested positive for SARS-CoV-2. Eighty-five percent of patients admitted to Edward Hospital in January 2022 were residents of DuPage or Will counties. COVID-19 vaccination rates for residents of DuPage and Will counties by age group are shown in Table 1.
Table 1: Primary Vaccination Rate in residents of DuPage and Will counties in Illinois through January 1, 2022
| County residence | Age Group | Not fully vaccinated | Fully vaccinated no booster | Booster vaccine |
|---|---|---|---|---|
| Will | 18-64 years | 29.6% | 45.6% | 24.8% |
| ≥ 65 years | 11.6% | 28.1% | 60.3% | |
| DuPage | 18-64 years | 19.9% | 47.3% | 32.8% |
| ≥ 65 years | 5.90% | 24.2% | 69.9% |
Methods: This was a case control study of adult patients with COVID-19 admitted to Edward Hospital with severe disease during January 2022 and the association with vaccination status, age, immunosuppression, medical conditions, gender, and smoking. Disease severity was measured as the highest level of respiratory (oxygen) support required and hospital survival. The study was approved by the Edward-Elmhurst Health IRB.
Inclusion and exclusion criteria: Inclusion criteria were: age 18 years or older, a date of admission to Edward Hospital in January 2022, and a positive SARS-CoV-2 viral test collected ≤ 20 days prior to admission or during admission. Patients with a previous positive viral test collected 21 to 90 days prior to admission were excluded. Patients admitted only to obstetrics or behavioral health units were excluded as they were predominantly hospitalized for conditions unrelated to COVID-19.
Risk Factors Evaluated
Vaccination status: Vaccination status was classified as (1) not fully vaccinated, (2) fully vaccinated but no booster, or (3) fully vaccinated plus a booster. Fully vaccinated was defined as having received either two mRNA vaccines, one Janssen vaccine, or a WHO-approved vaccine series > 14 days prior to the onset of symptoms or a positive test. Booster vaccinated was defined as being fully vaccinated plus ≥ 1 additional m-RNA vaccine administered > 14 days prior to onset of symptoms or positive test. Immunocompromised patients who received a third mRNA vaccine as part of their primary series were counted as booster vaccinated.
Age: Age in years was recorded as categorical variables, as follows: (1) 18–49, (2) 50–64, (3) 65–74, and (4) ≥ 75 years.
Gender: Gender of each patient was recorded as male or female.
Body mass index: Body mass index (BMI) in kg/m2 was measured and recorded as categorical variables as follows: (1) ≤ 24.9, (2) 25.0–29.9, (3) 30.0–34.9, (4) 35.0–39.9, and (5) ≥ 40.0.
Other risk conditions: Patients were assessed for immunocompromised status (none, stage 3 HIV, hematologic malignancy on treatment, receiving B-cell-depleting agent, organ transplant recipient, other malignancies on chemotherapy, and being on steroids or other immunosuppressive medications for > 14 days prior to the onset of COVID-19 symptoms); liver cirrhosis (none, or cirrhosis stage A, B, or C); chronic kidney disease (CKD) (none, CKD stage 1–2, CKD stage 3–5); chronic lung disease (none, chronic lung disease and not on home oxygen, or chronic lung disease and receiving home oxygen). Presence or absence of asthma, cardiac disease, diabetes mellitus, hypertension, neurologic disease, pregnancy, sickle disease, and smoking status (none, former, or active).
Duration of illness assessment: (1) Days from the onset of symptoms to admission and (2) days from the first positive test to admission were recorded.
COVID-19 disease severity outcome variables: Disease severity was assessed as the highest level of supplemental oxygen requirements maintained for > 24 hours or prior to discharge, 29-day survival, and survival at discharge. Oxygen requirements were categorized as (1) room air only (RA), (2) low-flow nasal cannula (NC) with radiologic evidence of pneumonia, (3) high-flow (HF) humidified oxygen at ≥ 15 L or high velocity, (4) noninvasive ventilation (NIV) or bi-level positive airway pressure (BiPAP), or (5) mechanical ventilation (MV).
Case Definitions for COVID-19 Severity Outcomes
- Any supplemental oxygen requirement in patients not on home oxygen
- Cases are patients who required any level of supplemental oxygen (NC, HF, NIV, MV).
- Controls are patients without oxygen requirements (RA).
- High-level oxygen requirement
- Cases are patients who required high-level oxygen (HF, NIV, or MV).
- Controls are patients with no oxygen requirements or low-flow nasal cannula.
- Mechanical ventilation or hospital death
- Cases are patients who received mechanical ventilation or died during hospital admission.
- Controls are patients who did not receive mechanical ventilation and were discharged from the hospital alive.
Results
Vaccination status and timing of vaccination: Fully vaccinated status was established for 229 patients based on doses recorded from the Illinois state database or provider documentation in the medical records. The last vaccine dose recorded was given < 5 months prior to admission for 83 of 85 patients who had received a booster and for 16 of 144 patients who had not received a booster. A total of 162 patients were categorized as not fully vaccinated based on both a lack of recorded doses from the state database and provider documentation of not being fully vaccinated. An additional two patients categorized as not fully vaccinated had no recorded doses and no documentation of vaccination status in their medical records.
Vaccination status, age, and immunosuppression: Booster vaccinated patients were more often immunocompromised and older than vaccinated patients without boosters. Patients not fully vaccinated were younger and less often immunocompromised than patients who were fully vaccinated, as shown in Table 2.
SARS-CoV-2 testing and duration of illness prior to admission: Days from the onset of symptoms and from the first positive test were longer in patients requiring oxygen than in patients on room air, as shown in Table 3.
Table 2: Vaccination Status, age, immunosuppression, and timing
| Pairwise analysis Age, BMI, Immunosuppression, timing last vaccine vs vaccine status | Not fully vaccinated | Fully vaccinated no booster | Booster vaccine | |
|---|---|---|---|---|
| Cases (N) | 164 | 144 | 85 | |
| Age (years) | Mean [95% CI] | 60.42 [57.78-63.06] | 66.78 [64.07-69.5] | 72.52 [69.78-75.26] |
| Median [25-75% IQ] | 61.5 [50-73.25] | 68 [58-79] | 74 [68-81] | |
| Immunocompromised (N) [% of group] | Immunocompromised | 14 [8.5%] | 20 [13.9%] | 26 [30.6%] |
| Not immunocompromised | 150 [91.5%] | 124 [86.1%] | 59 [69.4%] | |
| BMI (kg/m2) | Mean [95% CI] | 31.57 [30.17-32.97] | 29.35 [28-30.69] | 30.69 [28.9-32.49] |
| Median {25-75% IQ] | 30.5 [26-35] | 28 [23-35] | 29 [24-36] | |
| Last vaccine vaccine dose [% of group] | 2 weeks-4 months | NA | 16 [11%] | 83 [97.6%] |
| 5-11 months | NA | 128 [89%] | 2 [2.4%] |
Table 3: Oxygenation status by symptom onset and length of hospital stay
| Pairwise analysis Days from onset of illness Length of hospital stay | No O2 or NC if on home O2 | Nasal canula if not on home O2 | High Flow, Noninvasive, or Mechanical Ventilation | |
|---|---|---|---|---|
| Cases (N) | 255 | 80 | 58 | |
| Days from symptom onset to admit (Mean [95% CI) | Mean [95% CI] | 7.93 [6.99-8.87] | 9.24 [8.11-10.37] | 8.74 [7.58-9.91] |
| Cases with symptom history (316): No O2 (197), NC (76), high level (43) | Median [25-75% IQ] | 7 [3-11] | 9 [6-12] | 8 [6-10] |
| Days form 1st pos viral test to admit | Mean [95% CI] | 3.56 [2.9-4.22] | 4.82 [3.62-6.02] | 4.72 [3.14-6.31] |
| Median [25-75% IQ] | 0 [0-6] | 4 [0-8] | 2.5 [0-7] | |
| Length of hospital stay (days) | Mean [95% CI] | 3.87 [3.44-4.3] | 5.7 [5.02-6.38] | 15.5 [12.44-18.35] |
| Median {25-75% IQ] | 3 [2-5] | 5 [4-7] |
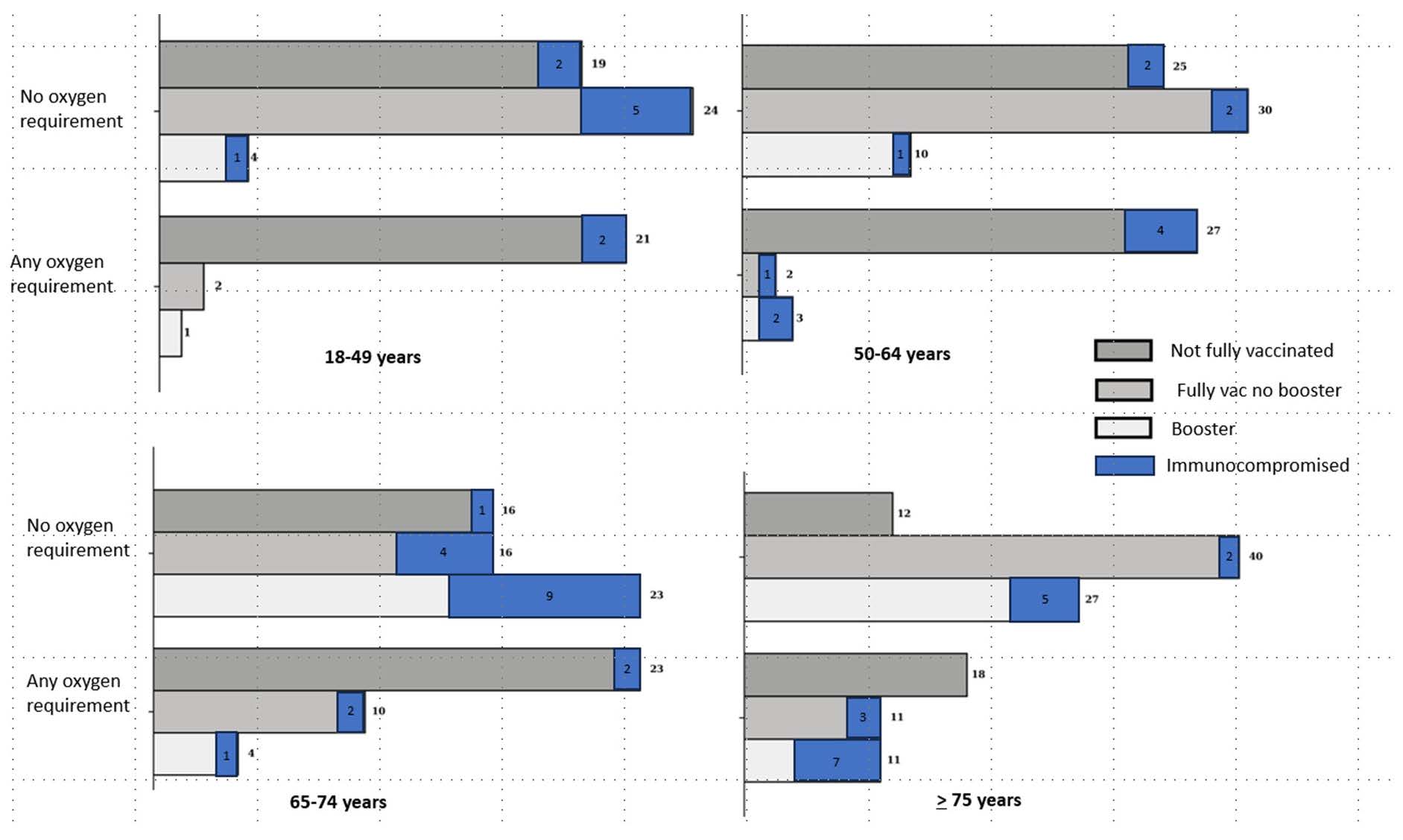
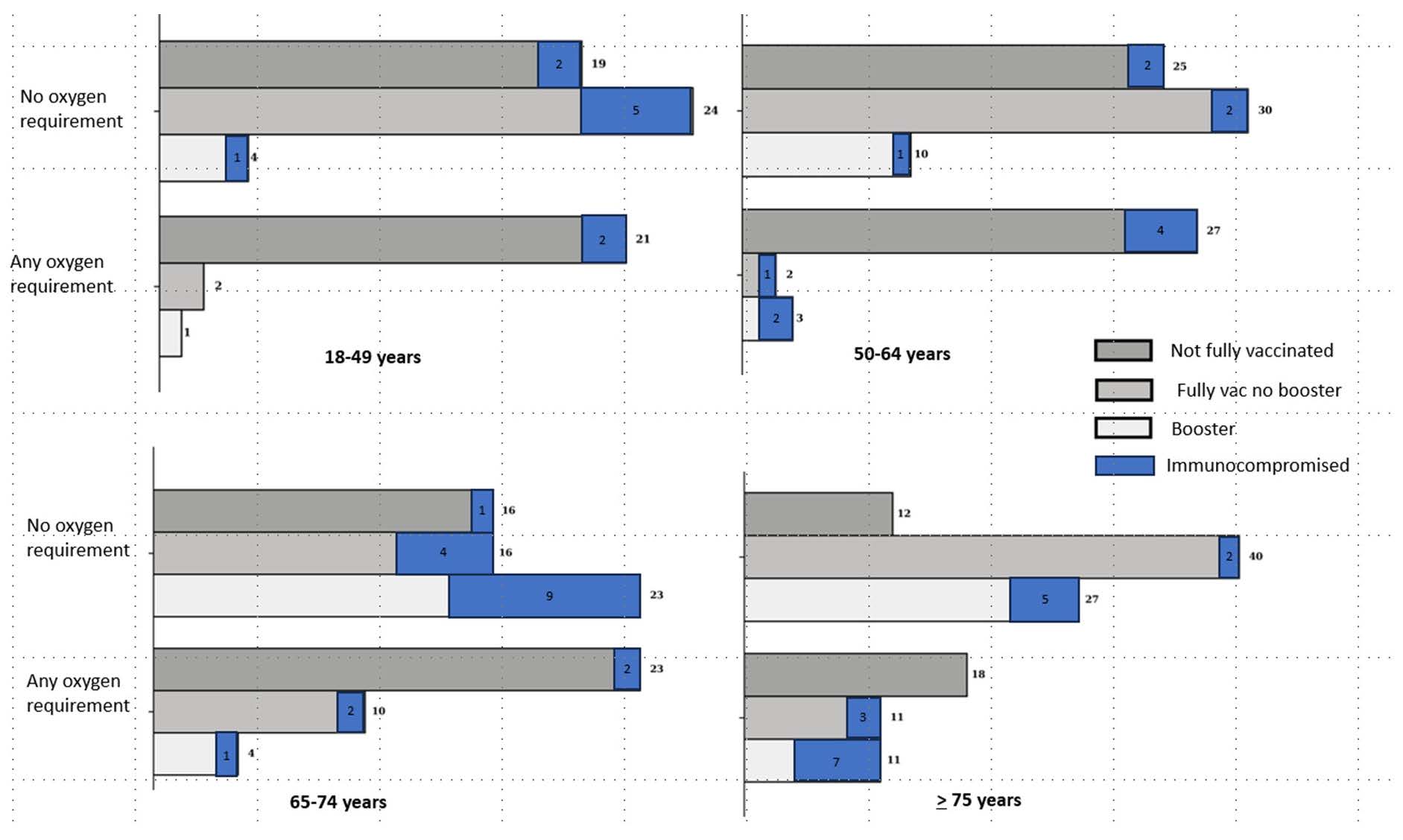
Supplemental oxygen requirement by age group, vaccination status, and presence of immunocompromised condition: Among patients aged 18–64 years, 48 of 56 (86%) who required oxygen, and 44 of 112 (39%) who did not require oxygen were not fully vaccinated. Among patients aged 65 years and older, 41 of 77 (53%) who required oxygen and 28 of 134 (21%) who did not require oxygen were not fully vaccinated. An immunocompromised condition was present in 24 of 133 (18%) who required oxygen and in 34 of 246 (14%) who did not require oxygen. In fully vaccinated patients, an immunocompromised condition was present in 16 of 44 (36%) who required oxygen and in 29 of 174 (17%) who did not require oxygen. (Figure 3)
Severe Outcome Measures
Of the 393 patients in our study, 379 had not been on home oxygen before admission. Oxygen requirements for patients not on home oxygen were: low flow nasal cannula (NC) in 80 patients, high flow (HF) in 24, NIV or BIPAP in 8, and mechanical ventilation (MV) in 21, and no supplemental oxygen required (RA) for 246 patients. Among the 14 patients on home oxygen before admission, the highest oxygen requirements were low-flow nasal cannula for 9, high-flow oxygen for 2, NIV for 2, and MV for 1. Twenty-eight patients died prior to discharge, including 15 of 22 patients on mechanical ventilation.
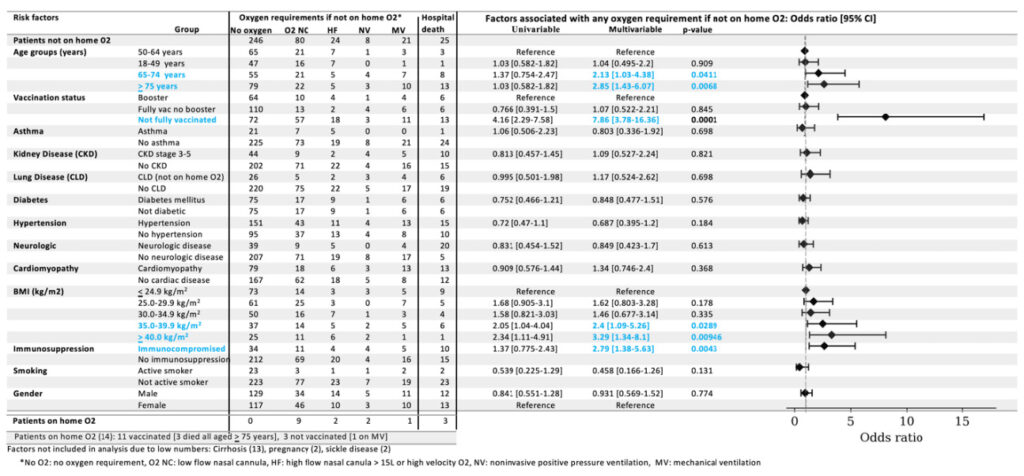
In a multivariable logistic regression analysis (Table 4), factors associated with any oxygen requirements in patients not on home oxygen were: (1) age of 65–74 years (odds ratio [OR] 2.13, 95% CI 1.03–4.38), age ≥ 75 years (OR 2.85, 95% CI 1.43–6.07), compared to 50–64 years; (2) being not fully vaccinated compared to booster vaccinated (OR 7.86, 95% CI 3.78–16.36); (3) obesity, with BMI 35–39.9 kg/m2 (OR 2.4, 95% CI 1.09–5.26), BMI ≥ 40.0 kg/m2 (OR 3.29, 95% CI 1.34–8.1), compared to BMI ≤ 24.9 kg/m2; and (3) immunocompromised status (OR 2.79, 95% CI 1.28–5.63). Factors not associated were: being fully vaccinated without versus with a booster (OR 1.07, 95% CI 0.522–2.21); an age of 18–49 compared with that of 50–64 years (OR 1.04, 95% CI 0.495–2.2), and other conditions. (Table 4)
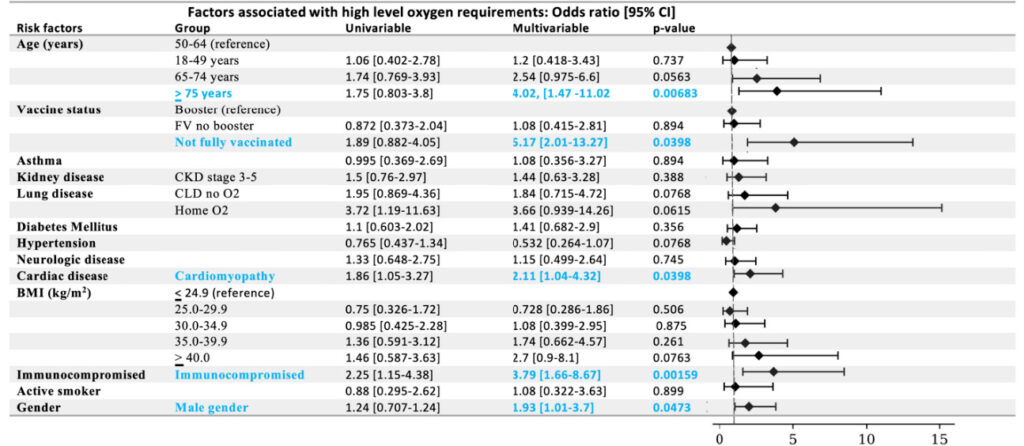
Factors associated with high-level oxygen requirements (HF, NIV, or MV) (Table 5) were: (1) age ≥ 75 years compared to age 50–64 years (OR 4.02, 95% CI 1.47–11.02); (2) being not fully vaccinated compared with being booster-vaccinated (OR 5.17, 95% CI 2.01–13.27); (3) cardiomyopathy (OR 2.11, 95% CI 1.04–4.32); (4) immunocompromised status (OR 3.79, 95% CI 1.66–8.67); and (4) male gender (OR 1.93, 95% CI 1.01–3.7). Factors not associated with high-level oxygen requirements were (1) being fully vaccinated without versus with a booster (OR 1.08, 95% CI 0.415–2.81); (2) an age of 18–49 compared with that of 50–64 years (OR 1.2, 95% CI 0.418–3.43); and other conditions.
Factors associated with the composite of MV or hospital death (Table 6) were (1) age ≥ 75 years compared to 50–64 years (OR 5.68, 95% CI 1.49–21.72); (2) being not fully vaccinated compared to being booster vaccinated (OR 5.21, 95% CI 1.63–16.61); (3) CKD stage 3, 4, or 5 (OR 3.17, 95% CI 1.27–7.96); (4) cardiomyopathy (OR 2.67, 95% CI 1.11–6.42); and (5) immunocompromised status (OR 4.63, 95% CI 1.72–12.5). Factors not associated were (1) an age of 18–49 compared to 50–64 years (OR 0.355, 95% CI 0.0337–3.75); (2) being fully vaccinated without a booster versus with a booster (OR 0.992, 95% CI 0.328–3.0); and other conditions.
Discussion
From December 2021 through January 2022, there was a surge of COVID-19 related hospitalizations in the United States due to the emergence of the Omicron variant. Prior to the Omicron period, there was a substantial population that was both unvaccinated and not previously infected [2]. January 2022, a period before widespread infection-related immunity, provided a window in which to study the impact of vaccination status and other risk factors on disease severity in Omicron infections.
This study included 393 patients admitted to Edward Hospital during January 2022 with COVID-19. Among 379 patients not on home oxygen, 133 required oxygen or mechanical ventilation. Among all 393 patients, 58 required either high-flow oxygen, non-invasive ventilation, or mechanical ventilation. Twenty-eight patients expired prior to discharge, including 15 of 22 who had been on mechanical ventilation. In the multivariable logistic regression analysis, not being fully vaccinated was associated with 7-fold higher odds of requiring supplemental oxygen. Other factors associated with requiring oxygen were immunocompromised status, age ≥ 65 years, and a BMI ≥ 35.0 kg/m2. Factors associated with high-level oxygen requirements and the composite of mechanical ventilation or hospital death were age ≥ 75 years, not being fully vaccinated, immunocompromised status, and cardiomyopathy. Factors not associated with requiring oxygen, high-level oxygen, or the composite of mechanical ventilation or hospital death were being aged 50–64 years compared with 18–49 years and not receiving a booster if fully vaccinated.
There is a wide body of evidence for the effectiveness of boosters on top of being fully vaccinated against COVID-19 related emergency department visits, hospitalizations, and deaths during the early Omicron period [3,4]. Vaccine effectiveness in preventing COVID-19 related hospitalization among participants in the IVY network during the BA.1 and BA.2 periods was higher in persons who received three mRNA vaccinations, 74–84%, than those who received two mRNA vaccinations, 46–75%, if the last vaccine dose was within four months. After five months, vaccine effectiveness was significantly diminished in both groups [5]. In a cross-sectional study of US adults hospitalized with COVID-19 from January through April 2022, COVID-19 associated hospitalizations were 10.5 times higher in unvaccinated persons and 2.5 times higher in vaccinated persons with no booster dose compared with those who received a booster [3].
Improved protection among booster recipients during the early Omicron period stems from higher levels and broader breadth of neutralizing antibodies following a third compared to following a second mRNA vaccine as well as more recent vaccination in booster recipients. Yet despite declines in neutralizing antibodies over six months following a second mRNA vaccine, memory B cells expand, and T cells remain stable [6,7]. This is thought to protect against progression from mild/moderate to severe disease [8]. In our study of patients hospitalized with COVID-19 during January 2022, the receipt of a booster among fully vaccinated patients was not associated with lower odds for severe respiratory disease. Taken together, this suggests that during the early Omicron period, the added protection of boosters on top of being fully vaccinated was predominantly in restoring protection against the early stages of infection rather than adding to the already strong protection against progression to severe pulmonary disease. Immune memory appears to play a major role in accounting for lower disease severity in Omicron infections. This is consistent with declining hospital mortality rates (Figure 4) [8] with rising population immunity [2] over the first year of the Omicron variant period.
Author Contributions
Conceptualization, J.P and J.P.; methodology, J.P, M.A., and J.P.; formal analysis, J.P. and J.P.; data curation, J.P. and M.A.; writing—review and editing, J.P, M.A., I.C. and J.P.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hermens, J.M.; Kesmir, C. Role of T cells in severe COVID-19 disease, protection, and long term immunity. Immunogenetics 2023, 75, 295–307. [CrossRef] [PubMed]
- DeCuir, J.; Surie, D.; Zhu, Y.; Gaglani, M.; Ginde, A.A.; Douin, D.J.; Talbot, H.K.; Casey, J.D.; Mohr, N.M.; McNeal, T.; et al. Effectiveness of Monovalent mRNA COVID-19 Vaccination in Preventing COVID-19-Associated Invasive Mechanical Ventilation and Death Among Immunocompetent Adults During the Omicron Variant Period-IVY Network, 19 US States, February 1, 2022-January 31, 2021. MMWR Morb. Mortal. Wkly. Rep. 2023, 72, 463–468. [CrossRef] [PubMed]
- COVID Data Tracker. Centers for Disease Control and Prevention. Updated February 19, 2022. Accessed February 19, 2022.
- Jones, J.M.; Manrique, I.M.; Stone, M.S.; Grebe, E.; Saa, P.; Germanio, C.D.; Spencer, B.R.; Notari, E.; Bravo, M.; Lanteri, M.C.; et al. Estimates of SARS-CoV-2 Seroprevalence and Incidence of Primary SARS-CoV-2 Infections Among Blood Donors, by COVID-19 Vaccination Status—United States, April 2021–September 2022. MMWR Morb. Mortal. Wkly. Rep. 2023, 72, 601–605. [CrossRef] [PubMed]
- Havers, F.P.; Pham, H.; Taylor, C.A.; Whitaker, M.; Patel, K.; Anglin, O.; Kambhampati, A.K.; Milucky, J.; Zell, E.; Moline, H.L.; et al. COVID-19-Associated Hospitalizations Among Vaccinated and Unvaccinated Adults 18 Years or Older in 13 US States, January 2021 to April 2022. JAMA Intern. Med. 2022, 182, 1071–1081. [CrossRef] [PubMed]
- Surie, D.; Bonnell, L.; Adams, K.; Gaglani, M.; Ginde, A.A.; Douin, D.J.; Talbot, H.K.; Casey, J.D.; Mohr, N.M.; Zepeski, A.; et al. Effectiveness of Monovalent mRNA Vaccines Against COVID-19–Associated Hospitalization Among Immunocompetent Adults During BA.1/BA.2 and BA.4/BA.5 Predominant Periods of SARS-CoV-2 Omicron Variant in the United States—IVY Network, 18 States, December 26, 2021–August 31, 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 1327–1334. [PubMed]
- Maringer, Y.; Nelde, A.; Schroeder, S.M.; Schuhmacher, J.; Hörber, S.; Peter, A.; Karbach, J.; Jäger, E.; Walz, J.S. Durable spike-specific T cell responses after different COVID-19 vaccination regimens are not further enhanced by booster vaccination. Sci. Immunol. 2022, 7, eadd3899. [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. COVID Data Tracker. Updated September 9, 2023. Accessed September 25, 2023.]

