Introduction
Epstein-Barr virus (EBV) is a member of the herpesvirus family (human herpesvirus 4) and is the primary causative agent of infectious mononucleosis. Initial presentation of infection includes low-grade fevers along with malaise, which later develops into tonsillitis and/or exudative pharyngitis and cervical node enlargement. Approximately 90% to 95% of adults are EBV-seropositive with the majority of infections being asymptomatic. In this case report, we discuss a rare and intriguing manifestation of hepatitis attributed to EBV. Mild elevations of transaminases are commonly seen but severe hepatitis with jaundice is rare [1]. This infrequent complication is characterized by a cholestatic pattern of liver injury with direct hyperbilirubinemia. With a reported incidence of jaundice at just 6.6% in the severe hepatitis population [1], our case stands out given our patients presentation with periorbital jaundice. We discuss the atypical presentation of hepatitis and the importance of a multidisciplinary approach to determine effective management.
Case Presentation
We present a case of a 48-year-old male with a medical history of asthma, hypertension, dyslipidemia and mood disorder, who presented to the hospital for intermittent fevers and malaise. Two days prior to admission he was evaluated at an urgent care facility for progressively worsening fever, chills, malaise and periorbital jaundice. He sequentially developed mild swelling of his throat and described the sensation of his uvula being displaced. He was advised to present to the emergency department after labs at the urgent care demonstrated elevated transaminases and urinary bilirubin. Recent travel history included weekly travel for 8 weeks in a row, which likely exposed the patient to individuals with communicable illnesses. Pertinent labs on admission notable for transaminitis were aspartate aminotransferase, 299 IU/L; alanine aminotransferase, 528 IU/L; hyperbilirubinemia, 8.3 mg/dL; elevated gamma-glutamyl transferase, 1154 IU/L; positive immunoglobulin M (IgM) and immunoglobulin G (IgG) for EBV; and leukocytosis with marked lymphocytosis. Imaging including ultrasonography and computed tomography of the abdomen and pelvis revealed fatty liver and splenomegaly.
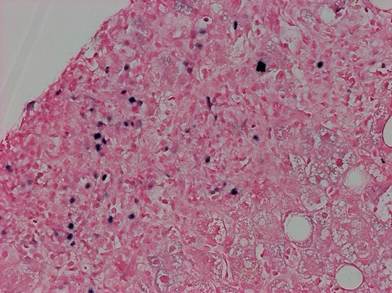
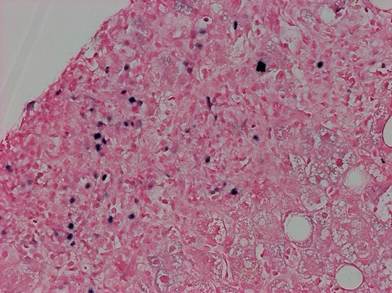
The patient remained tachycardic, dyspneic and febrile throughout the initial few days of hospitalization. Specific viral serology demonstrated positive EBV viral capsid antigen (VCA) IgM with negative EBV nuclear antigen IgG. On day 6 of hospitalization, the patients EBV polymerase chain reaction (PCR) returned with a positive result of 116,000 copies. After discussion between Infectious Disease, Gastroenterology and the hospitalist team, it was determined the patient would benefit from liver biopsy to distinguish between primary EBV infection, viral hepatitis and drug-induced liver injury. Liver biopsy demonstrated chronic inflammation of the portal tracts with atypical T cells and scattered medium-sized B cells, of which many are positive for EBER-ISH (Epstein-Barr encoding region in situ hybridization) confirming primary EBV hepatitis (Figure 1). This test is highly sensitive and specific and is considered the gold standard for detecting EBV-encoded small RNAs that are abundantly expressed in latently infected cells.
Towards the end of his hospitalization, the patient developed a new rash which likely was a delayed manifestation of EBV. Risks and benefits were discussed with the patient and he was started on a short course of corticosteroids. Following initiation of steroids, he reported significant improvement of symptoms alongside increased appetite and ability to ambulate without fatigue. He was stable for discharge on day 10 of hospitalization with a prescription of prednisone (total 7-day course). The patient followed up in the Infectious Disease clinic for 3 months after discharge from the hospital. During that time, EBV PCR levels were regularly monitored and demonstrated a downward trend from 8900 to 413 copies, ultimately falling below 200 copies.
Discussion
The findings of this case highlight the significance of considering EBV as a potential etiological agent in cases of hepatitis and underscores the importance of timely diagnosis and management in achieving favorable patient outcomes. EBV typically presents as a prodrome of fatigue along with low-grade fevers followed by lymphadenopathy, generalized weakness/myalgias and exudative pharyngitis. Mild elevations in aminotransferases are frequently seen in the first 3 weeks of symptomatic infections, whereas approximately 10% of the population have more severe symptomatic hepatitis. Our case underscores the uncommon presentation of cholestatic liver changes, as only 3% of patients exhibit serum bilirubin levels exceeding 8 mg/dL [1]. The cholestatic pattern of injury observed is theorized to arise from the direct impact of the proinflammatory cytokines from the virus on the sinusoidal and canalicular transporting systems [2]. Just as seen with our patient, labs typically demonstrate leukocytosis with atypical lymphocytes and detection of EBV specific serology [3]. Definitive biopsy results demonstrate a string of beads pattern of lymphocytic sinusoidal infiltrate. The expansion of portal tracts seen on biopsy is due to a lymphocytic infiltrate which consists of reactive cytotoxic T cells, natural killer cells and EBV-infected B cells [3]. Treatment is primarily supportive care with nonsteroidal anti-inflammatory drugs and/or acetaminophen. There is limited clinical data to support using acyclovir, as antivirals have only shown suppression of salivary EBV shedding. Antiviral medications do not reduce the replication of EBV or significantly reduce duration of clinical symptoms [4]. Historically, corticosteroids have been used to manage pharyngeal inflammation and prevent airway obstruction. The literature regarding steroid use for symptomatic treatment reveals conflicting outcomes and results have been variable on a case-by-case basis. In our patients case, we considered the fever and systemic symptoms to support the immune-mediated response as the driver of his symptoms, especially when accounting for his age. The decision to start the patient on prednisone 40 mg daily for a 7-day course proved beneficial in our patients case as he reported improved appetite, decreased fatigue and overall improvement of symptoms. While clinicians commonly see the typical manifestations of primary EBV infection, encountering EBV hepatitis is rare. When considering serologic testing, IgM antibody to VCA is the most useful for acute infection, as elevated titers are present during the first 2–3 months of disease. However, IgG antibody to VCA is often a marker used to assess prior exposure [5]. In most cases, individuals exhibit serologic evidence of EBV exposure during young adulthood. Yet in our case, the patient experienced primary infection at age 48, potentially elucidating the severity of his condition. Keeping in mind the variability of EBV manifestations, it is important to make treatment decisions that are supported by clinical data and to have the ability to modify them to enhance symptom management.
Conclusions
We presented a case with the uncommon manifestation of primary Epstein-Barr virus hepatitis alongside the common symptoms of the disease in an immunocompetent individual. Biopsy typically shows lymphocytic portal infiltrates with labs demonstrating a cholestatic pattern of liver injury. This case underscores the commonly underestimated contribution of EBV to hepatitis, emphasizing the importance of thoroughly evaluating all patient symptoms and customizing treatment on an individual basis.
Author Contributions
Conceptualization, methodology, investigation, resources, writing—original draft preparation, writing—review and editing, and visualization completed by both authors equally. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
N/A.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Méndez-Sánchez, N.; Aguilar-Domínguez, C.; Chávez-Tapia, N.C.; Uribe, M. Hepatic manifestations of Epstein-Barr viral infection. Ann. Hepatol. 2005, 4, 205–209. [PubMed]
- Manappallil, R.G.; Mampilly, N.; Josphine, B. Acute hepatitis due to infectious mononucleosis. BMJ Case Rep. 2019, 12, e229679. [CrossRef] [PubMed] [PubMed Central]
- Schechter, S.; Lamps, L. Epstein-Barr Virus Hepatitis: A Review of Clinicopathologic Features and Differential Diagnosis. Arch. Pathol. Lab. Med. 2018, 142, 1191–1195. [CrossRef]
- Hellwig, T.; Jude, K.; Meyer, B. Management Options for Infectious Mononucleosis. US Pharm. 2013, 38, 38–41.
- Cohen, J.I. Epstein-Barr virus infections, including infectious mononucleosis. In Harrisons Principles of Internal Medicine, 21st ed.; Loscalzo, J., Fauci, A.S., Kasper, D.L., Hauser, S.L., Longo, D.L., Jameson, J.L., Eds.; McGraw Hill: New York, NY, USA, 2022; Volume 2.

